CONSUMER TIPTo get a better idea of what a procedure will cost from hospital to hospital, insured patients need to call both the hospital and their insurance company and ask for an estimate what their out-of-pocket expense will be based on their deductible and coinsurance, says Erlanger vice president of payer relations Steve Johnson.Medicare patients have fixed deductibles they should be aware of. Uninsured patients should speak with hospitals about discounts and payment plans ahead of time.
There's one clear fact about the murky, ever-shifting world of hospital charges:
They always get higher.
And the speed with which they can rise is revealed in a trove of new Medicare data, released last week, that shows how much hospitals across the nation bill for their most common procedures.
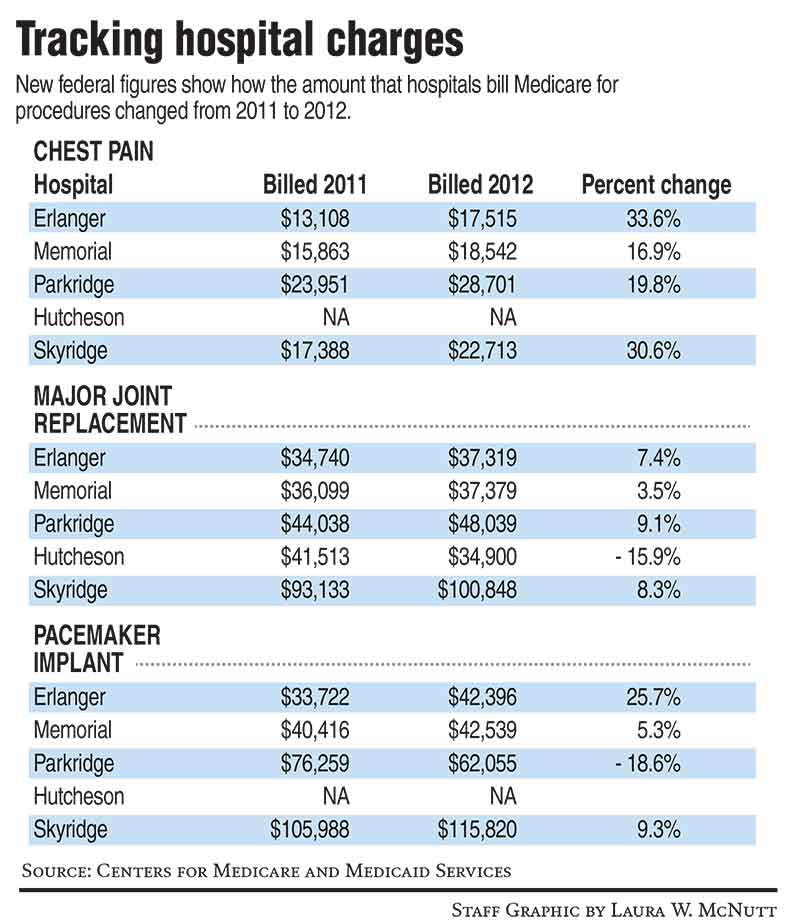
In the Chattanooga region, for example, hospitals increased charges for most of their treatments between 2011 and 2012 -- by 10, 20 and even more than 30 percent, in some cases.
This is the second year that Medicare -- the federal health insurance program for people 65 or older -- has released the hospital billing data, which previously had been kept under wraps.
When the information was first publicized last year, it confirmed the wide variations in what different hospitals charged for the same procedure, including those in the tri-state region.
With the release of this year's data, those variations were once more underscored. In this region alone, there's a $73,400 price difference for the same pacemaker insertion offered by two hospitals just 30 miles from each other.
Besides tracking those kinds of disparities, the list of charges also makes it possible to track just how much charges for a procedure increase year to year.
A New York Times analysis of the data found that hospitals charged more for all of the procedures that could be compared to the prior year, and found that for all but seven, the rise in the charges exceeded the nation's 2 percent inflation rate that year.
Nationally, some of the biggest increases were for treating chest pain, with a 10 percent bump on average. Local hospitals reported significant increases for that treatment, from 16 to 33 percent.
For a few procedures, local hospitals lowered their charges.
Different hospitals have different philosophies in how they price, and there are many variables that lead to increases. But one absolute that impacts everyone is the rising cost of medical devices and drugs.
Market prices for services or room rates also tend to go up industrywide. Erlanger Health System uses a consultant to analyze what peer hospitals may be charging and make recommendations on how to consistently land in the midrange for pricing.
Medicare officials have said they are releasing the data as part of an effort to bring more transparency to health care costs.
Health experts say it gives a better picture of how health care pricing works -- but not a full one. There's still plenty of debate about what drives such stark variations and what's at the heart of rising health costs.
Hospitals argue that the release of the raw data has little practical value for consumers, who will usually never see -- much less pay -- "sticker price" for a procedure.
What patients actually pay has more to do with the type of coverage they have than the listed charges, a statement released by Parkridge Health System explained.
"Government programs like Medicare and Medicaid determine how much they reimburse hospitals. Insurance plans negotiate their payments."
Despite increases year to year, insurers, like BlueCross BlueShield of Tennessee, say they have buffers including multiyear contracts and rotating contract renewals to "mitigate the impact of yearly cost increases that would raise our members' premiums," said BlueCross spokeswoman Mary Danielson.
The uninsured, hospitals say, typically receive discounts or may receive charity care.
"[The data] is a step in the right direction for consumer engagement, but I worry it gets the consumer focused on the wrong thing," said Steve Johnson, vice president of government and payer relations for Erlanger.
"As a consumer, you're concerned about cost and quality. The charges don't show you that."
And at the end of the day, what hospitals actually get reimbursed by Medicare is a much smaller figure than what they charge, with markedly less variation.
In 2011 and 2012, SkyRidge Medical Center in Cleveland, Tenn., tended to have the region's highest Medicare charges. But what it actually received from the agency is in the same ballpark as what other local hospitals received, or even less.
"If you look at the average total payments to our hospital, you'll see they are comparable to what other hospitals in this area are paid and far less than what any hospital 'charges,'" said Coleman Foss, CEO of SkyRidge.
Medicare payments typically do not cover the actual cost of providing the care, he said.
But consumer advocates and health access activists say the data release marks an important shift in the health industry.
"It's all operated without transparency for so long, that hasn't worked as far as lowering inflation. We may not be seeing big impacts of transparency now, [but] I think in the long run, we will," said Michele Johnson, executive director of the Tennessee Justice Center, a public policy advocacy organization. She is unrelated to Steve Johnson.
Craig Becker, president of the Tennessee Hospital Association, also says that while the data release has little value for patients now, it signals long-term changes in the industry.
"It's just that it sensitizes people to the cost of hospital care, and it's making hospital leaders more aware and sensitive to what's on their own charge lists."
And that consumer engagement is likely to only increase.
The Affordable Care Act will bring even more changes to how hospitals are paid, tying reimbursement rates more closely to health outcomes, and pushing providers toward greater transparency and consumer involvement.
"Once you see the map emerging with quality and outcomes and pricing, you start seeing conversations about lowering pricing and improving outcomes," said Michele Johnson.
Contact staff writer Kate Harrison at kharrison@timesfreepress.com or 423-757-6673.